

Editorial Note. This research paper was initially submitted in December 2023 as part of the Master of Science in Global Healthcare Leadership programme at the University of Oxford. The programme is jointly offered by the Nuffield Department of Primary Care Health Sciences and Saïd Business School. It was prepared for Module 7: Challenges in Global Healthcare, taught by Professors Proochista Ariana and John Powell. Minor revisions have since been made to reflect further research conducted after the original submission.
Peter Bruegel, in 1567, set before the world a crowded canvas. Humanity pressed close. Figures bent by toil, play, and hunger; a tapestry of lives stitched together by custom and circumstance. His vision lingers over the ordinary, yet within the ordinary lies portent: bodies shaped by fate, food, and labour that sustain or undo them. To gaze upon his world is to glimpse our own in allegory.
Seated at the heart of Davidson County is Nashville, whose streets, kitchens, schools, and hospitals echo with the same human frailty and resilience. Bruegel’s observations remind us that, just as in his era, today’s ordinary lives in Nashville reflect larger challenges, specifically, the prevalence and impact of obesity across Davidson County and the state of Tennessee.
Here, amid the painted throng, we see how patterns of plenty and privation inscribe themselves on flesh. From the old painter’s stage, we step into the present crisis. A quiet epidemic of obesity, where metrics falter and policies wrestle with inequity, our health is weighed not only in pounds but in the future.
The Problem
Davidson County, Tennessee, USA, home to Nashville and its surrounding communities, is facing a growing public health crisis driven by obesity. The epidemic increasingly strains the county’s healthcare system and economic stability. Obesity is defined as excessive fat accumulation that poses health risks. Traditionally, it has been measured using the Body Mass Index (BMI), a simple calculation based on height and weight. The context of this study includes the prevalence of obesity in disadvantaged communities in Tennessee.
While BMI remains a convenient population-level tool, modern research has highlighted its serious limitations for assessing individual health. BMI cannot distinguish between muscle and fat, overlooks fat distribution, and does not adjust well across sex, age, or ethnicity. As a result, experts are increasingly recommending that BMI be supplemented or even replaced by more precise, individualised metrics.
To deal with obesity, it is recommended that Davidson County evaluate a range of strategic interventions directed toward multiple facets of the dilemma (see Table 1):
| Focus Area | Key Issues Addressed | Proposed Strategies | Target Outcomes |
|---|---|---|---|
| Obesogenic Food Environments | Unhealthy food availability, fast food prevalence | Policy revisions for healthier alternatives | Healthier food environments, reduced food insecurity |
| Economic Strategy & Industry Collaboration | Fiscal strain of obesity, unhealthy food marketing | Long-term models, healthier product collaboration | Sustainable change in the food system |
| Problematic Social Media Use (PSMU) | Influence on youth lifestyles | Educational campaigns on activity and nutrition | Reduced PSMU effects, improved youth health |
| Family Dynamics & Feeding Practices | Child nutrition shaped by family behaviour | Promoting responsive feeding and healthy parenting | Prevention of childhood obesity |
Note. This table summarises multi-sectoral strategies to address obesity-related challenges through environmental, economic, behavioural, and familial lenses.
Fostering sustainable, healthy food environments is an essential component of policy revisions targeting obesogenic settings. Within economic strategy, the fiscal burden of obesity is a key consideration, underscoring the importance of initiatives that collaborate with industry and aim to produce and market healthier food and drink options.
Regarding problematic social media use (PSMU), the original intervention framework emphasises physical activity and healthy eating as distinct focuses of educational campaigns. Each focus area contributes to reducing PSMU-related health risks. Family dynamics encompass more than behaviour alone, including interactions, relationships, and child-rearing practices. These shape a child’s nutritional choices and overall health. Psychosocial factors are critical to the prevention of childhood obesity and should be addressed explicitly in programme development and policy evaluation.
Economic Implications. The interventions for addressing unhealthy weight in Davidson County have short-term costs and long-term benefits. Initial investments in education, policy formulation, and infrastructure changes are compulsory for preserving improvements. In the long term, decreasing obesity prevalence will reduce healthcare costs, improve workforce productivity, and foster economic growth. Addressing obesity in Davidson County requires a comprehensive strategy that considers political, economic, and social factors. These efforts, while challenging, are essential for safeguarding Davidson County's long-term health and economic stability in the face of this growing public health crisis.
Policy Brief
Addressing the Burden of Obesity in Davidson County
Davidson County, Tennessee, is home to nearly 750,000 residents and faces an increasing burden of obesity and its associated diseases. County health officials recognise obesity as a multifaceted public health emergency, with implications for community health, healthcare system strain, and economic vitality. Davidson County (including Nashville) faces a significant local obesity burden: adult obesity stands at 24.7%, with an additional 37.4% overweight; 29% of adolescents self‑report being overweight.
The consequences of the disease extend beyond individual health, imposing substantial burdens on healthcare expenditures and workforce productivity. In this urban region, sedentary lifestyles in conjunction with dietary patterns have contributed to rising obesity rates. Marked by excessive fat accumulation, obesity is measured using the Body Mass Index (BMI). A BMI over 25 indicates overweight, and over 30 is classified as obesity (Zamora, A. 2012; See Figure 1).
Figure 1. Body Mass Index (BMI) chart illustrating male and female body types across standard BMI categories, from underweight to morbidly obese.
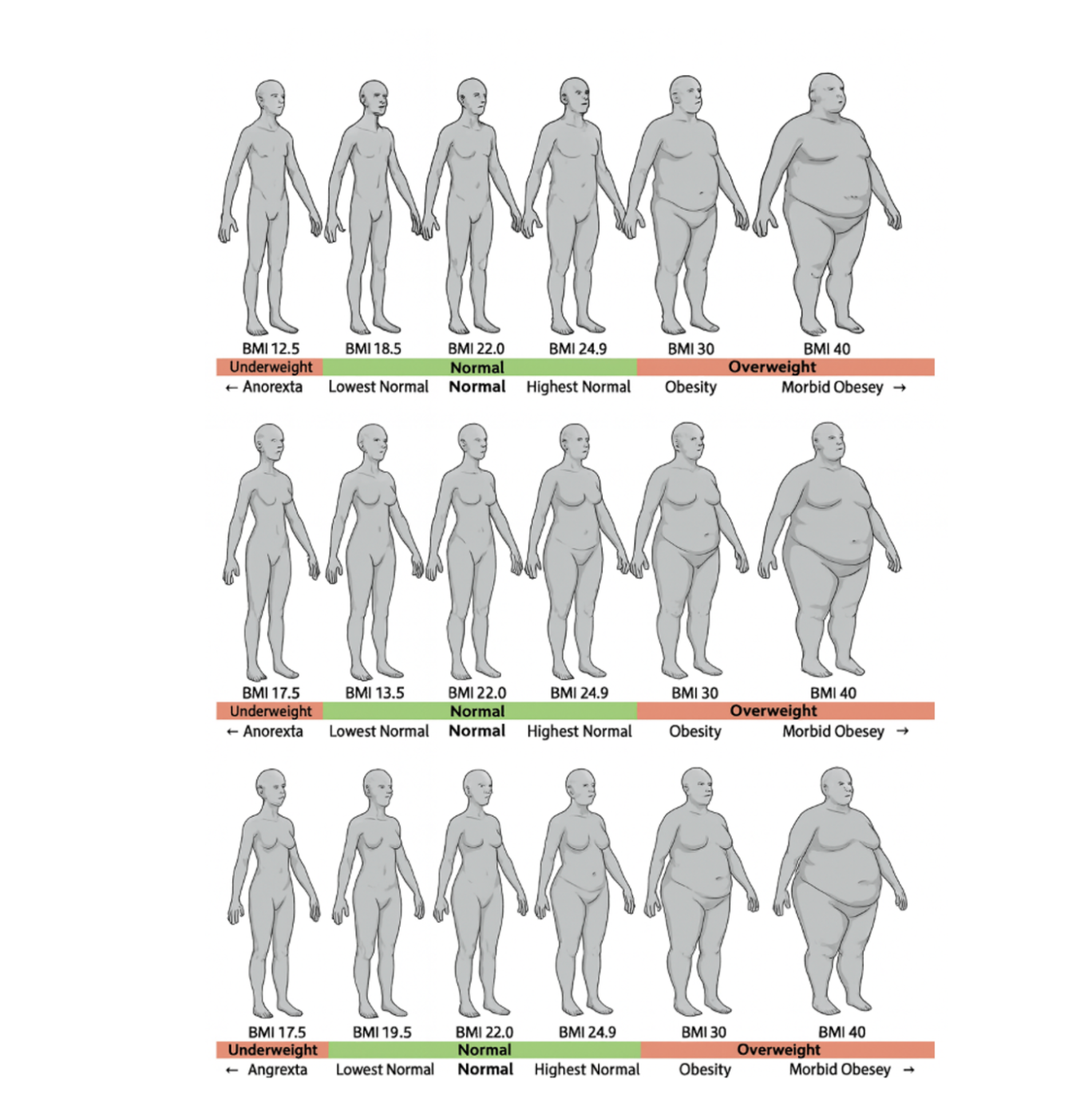
In Tennessee, about 37.6% of adults are obese (BMI ≥ 30), placing the state among the highest in the U.S. In Davidson County, 33% of adults are obese, and more than 22% of children aged 10–17 live with obesity. The prevalence of obesity has steadily risen over the past decades, mirroring national trends. The CDC estimates that obesity-related healthcare costs in Tennessee were $2.49 billion in 2014. According to the World Health Organization, overweight is defined as a Body Mass Index (BMI) ≥ 25 and obesity as a BMI ≥ 30.
"The worldwide prevalence of obesity has nearly tripled since 1975, mainly due to the adoption of a progressively more sedentary lifestyle and the consumption of less healthy diets."
At the U.S. national level, obesity is estimated to account for about 5–10% of total healthcare costs, a burden consistent with the substantial costs now observed in Tennessee.
The Problem
Child Obesity and Parental Feeding Practice. A systematic review by Hurley et al. (2011) emphasises the association between parental feeding practices and child obesity. In Davidson County, Tennessee, a high-income U.S. county where lifestyle and dietary practices are shaped by social and economic conditions, these insights are especially relevant. Responsive feeding practices constitute an important determinant of child weight outcomes. This finding, therefore, underscores the necessity of family-focused interventions in this context (Hurley et al., 2011). Importantly, this context-driven perspective is distinct from the genetic liability of obesity (Herle et al., 2022). Furthermore, Qiu et al. (2023) observed that “childhood inadequate eating behaviors contribute to the epidemic of obesity” (see Table 2).
Table 2. Mean ± SD for Parental Feeding Practices, Children Eating Behavior, and Food Preference (Qiu et al. (2023)

Food Environments and Food Insecurity.
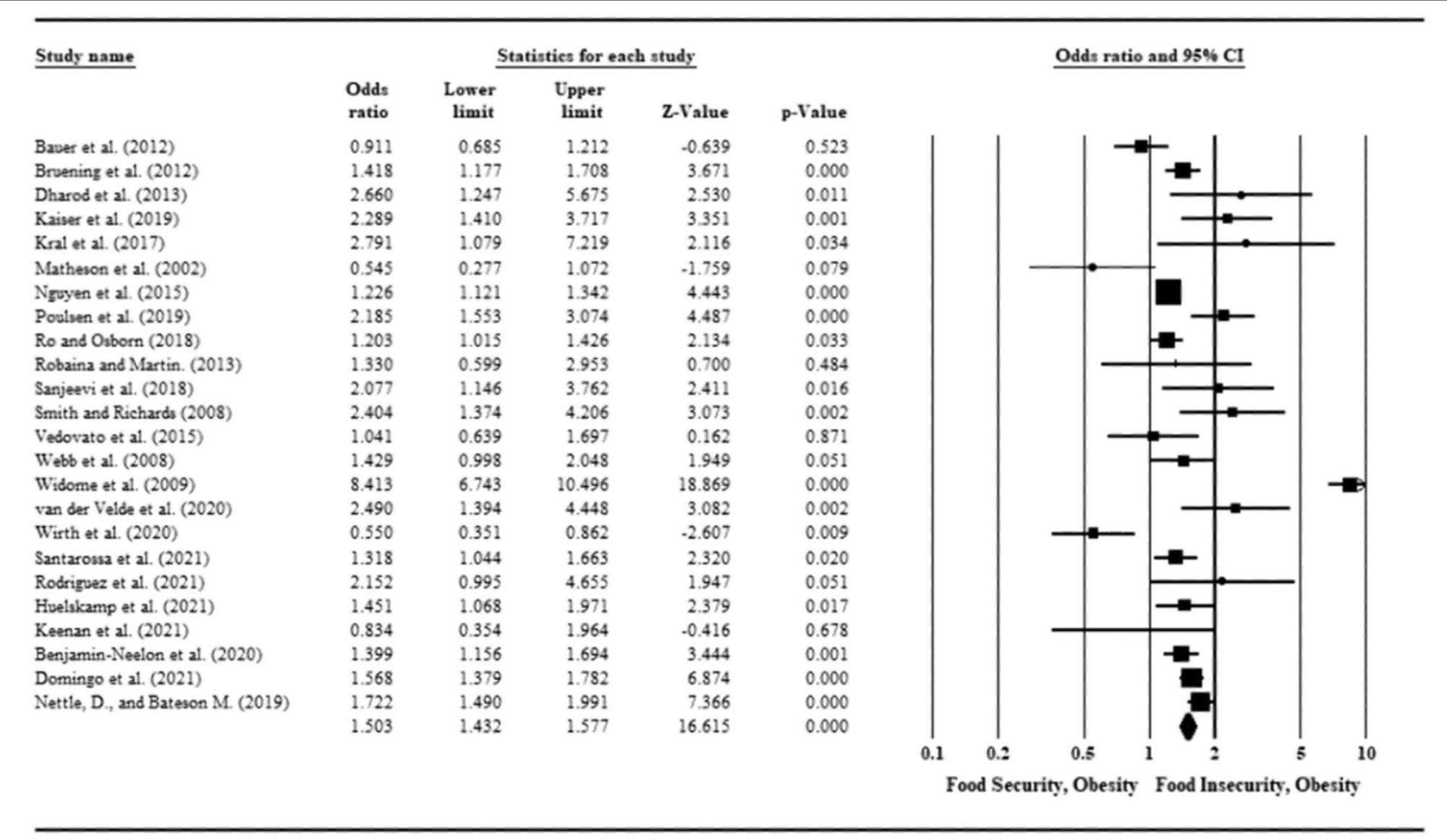
Eskandari et al. (2022) emphasise the role of obesogenic food environments in high-income countries, a factor highly relevant to our context. The prevalence of fast food and limited access to healthy options in metropolitan areas highlight the need for targeted structural and policy interventions (Eskandari et al., 2022). This is further substantiated by the meta-analytic evidence in Table 2, which demonstrates that individuals experiencing food insecurity are significantly more likely to be affected by obesity. Okunogbe, A. et al. (2022) concluded, “Food insecurity increased the risk of obesity among adults and children. Therefore, individuals experiencing food insecurity were more likely to be affected by obesity.”
Table 3. Forest plot showing odds ratios (ORs) with 95% confidence intervals for the association between food security status and obesity
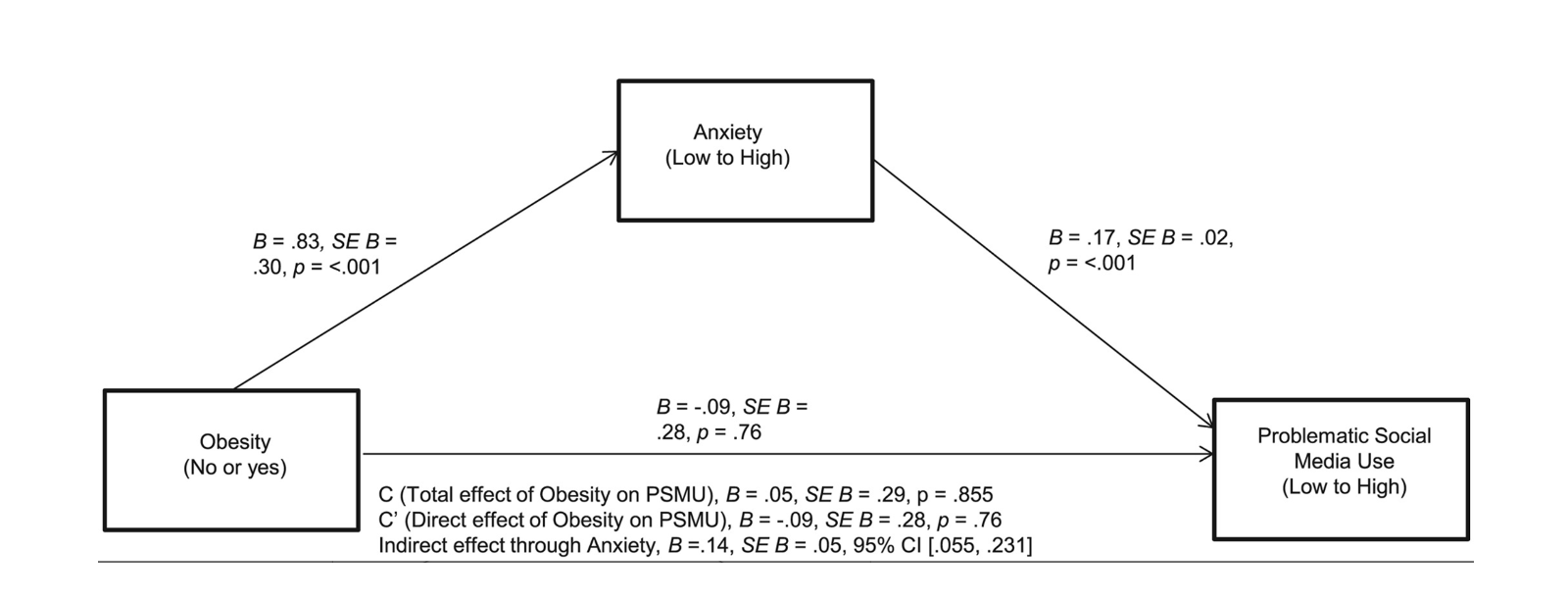
Research by Oduro et al. (2023) suggests a connection between PSMU and an increased risk of overweight/obesity among adolescents who are impacted by lifestyle habits such as physical inactivity. This is especially relevant in Davidson County, where internet and social media use is high among the youth, demonstrating the requirement for interventions that address media usage and facilitate healthy habits (Oduro et al., 2023). "The present study found a significant positive association between obesity and PSMU. Further, this study found that this relationship was mediated by both anxiety and depressive symptoms individually" (Jolliff, Moreno, & D'Angelo, 2020; see Figures 2 and 3).
Figure 2. A mediation model with unstandardized coefficients, controlling for the effect of depressive symptoms. Confidence intervals are shown. PSMU = problematic social media use.
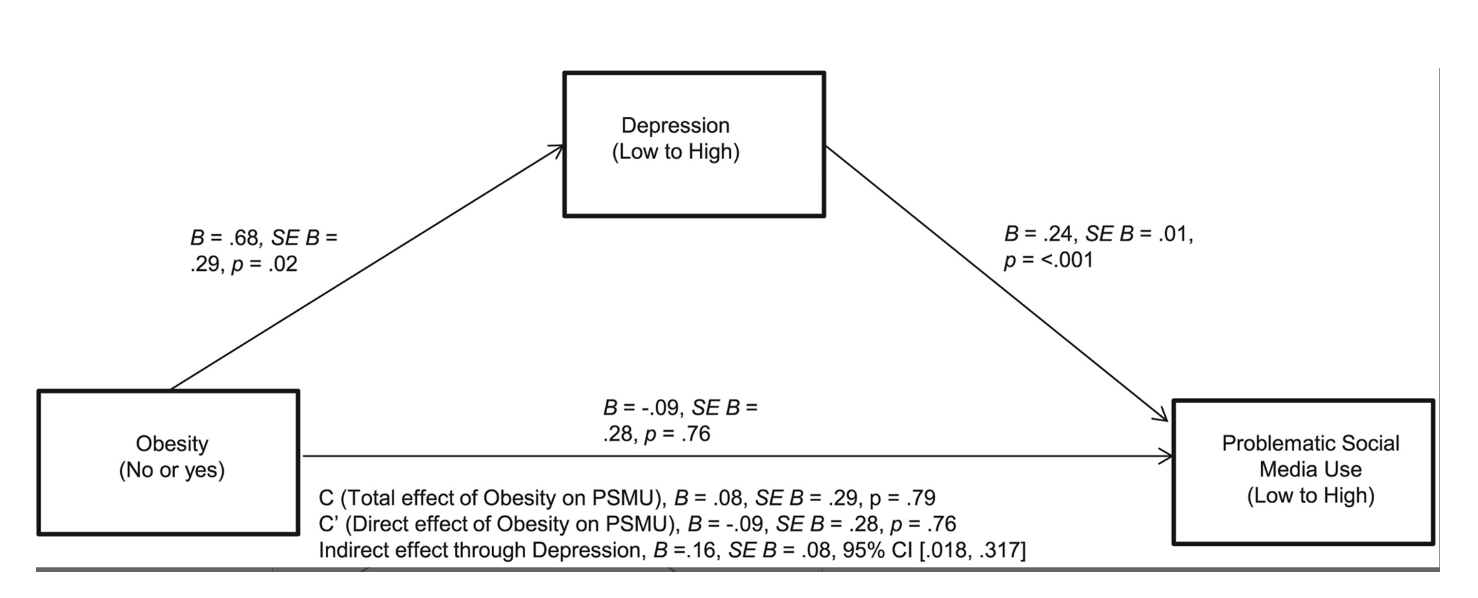
Figure 3. A mediation model with unstandardized coefficients, controlling for the effect of anxiety symptoms. Confidence intervals are shown. PSMU = problematic social media use.
The OECD reports that overweight and obesity could decrease GDP in its member countries by an average of 3.3% annually. This considerable economic burden is significant for Davidson County. This indicates that comprehensive public health strategies are necessary to address this issue (OECD). The study by Okunogbe et al. (2022) furnishes "novel evidence of the economic impact of [overweight and obesity] (OAO) across different economic and geographic contexts." (Okunogbe et al., 2022; see Figure 4).
Figure 4. Framework of cost components associated with overweight and obesity
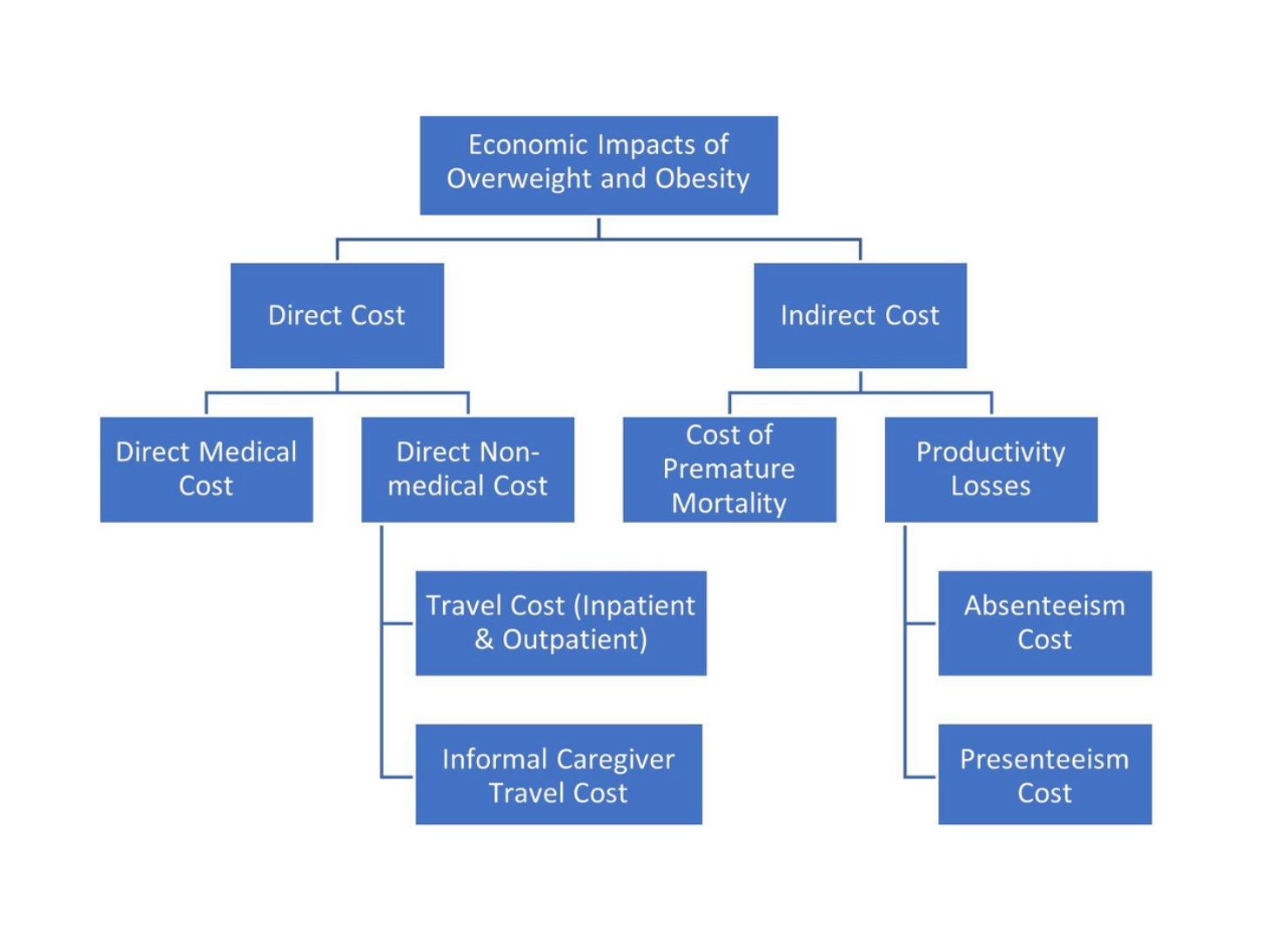
As Figure 4 illustrates the multifaceted cost components of obesity, it becomes clear that addressing this burden requires more than understanding economic impacts. To move from analysis to action, Davidson County has begun to outline intervention strategies aimed at reshaping environments, influencing behaviours, and fostering sustainable health improvements.
Intervention Strategies in Davidson County
Costs, Benefits, and Sectoral Influences
Obesogenic Food Environments
Regulatory changes and investments to improve access to nutritious foods carry initial costs. Long-term benefits include reduced healthcare spending and growth in health-conscious industries. These changes can foster innovation and stakeholder alignment.
Economic Planning & Collaboration
Policy development and negotiations with the food industry involve costs. The goal is reduced healthcare burden and industry innovation for a resilient, health-focused economy.
Family Dynamics & Feeding Practices
Programs and workshops focused on family education come with upfront costs. These efforts yield lasting healthcare savings and address obesity at its roots, building a healthier society.
Social Media Use & Adolescents
Educational campaigns require investment but can enhance adolescent physical and mental health. Benefits include better academic performance and long-term societal well-being.
While these intervention strategies highlight the immediate priorities and areas of focus, they also serve as building blocks for broader, more comprehensive approaches. The following section expands on these foundations, examining strategies for addressing obesity through a county-wide lens that integrates economic, social, and behavioural dimensions.
Strategies for Addressing Obesity
Evaluating the Economic Impact of Obesity Intervention Strategies in Davidson County: Costs, Benefits, and Sectoral Influences
Implementing interventions to address obesity in Davidson County carries costs and benefits, affecting diverse sectors of the economy. Here is a breakdown of the possible economic implications.
Obesogenic Food Environments and Food Insecurity.
Regulatory changes and investments to enhance accessibility to more nutritional food options involve certain costs. However, these costs are expected to yield significant benefits, including lowered long-term healthcare expenditures due to a healthier population. Moreover, health-focused sectors can mature as consumer demand shifts towards healthier products and services. The general consequence of these initiatives could lead to a significant change within the food industry, aligning diverse stakeholders towards creating healthier food environments. This alignment supports public health objectives and drives innovation and economic opportunities in the health and wellness sectors.
Economic Planning and Industry Collaboration.
The function of policy development and engaging in negotiations with the food and beverage industry incurs certain costs. These measures are directed towards developing a sustainable economy that experiences lower healthcare burdens due to improved public health. The industry has potential for innovation as it acclimates to new health-focused needs and regulations. By balancing the interests of public health and industry, these endeavours seek to establish a resilient, health-conscious economic environment.
Problematic Social Media Use (PSMU) and Adolescent Lifestyle Habits.
The creation of educational campaigns entails inevitable costs, but these investments are central to dealing with obesity-related health issues among adolescents. The merit of such campaigns expands beyond physical health with the potential to improve mental health and academic performance in young people. By educating adolescents on healthy lifestyle choices, these campaigns lay the groundwork for a healthier, more productive future generation, underpinning a broader strategy to enhance public health and societal well-being.
Family Dynamics and Responsive Feeding Practices.
Investing in educational programs and workshops involves certain costs, but these investments are necessary for reaching long-term health and economic benefits. By concentrating on lowering obesity rates, these educational endeavours can significantly decrease healthcare costs. The results of these programs are profoundly positive for the healthcare system and the workforce, aligning perfectly with the overarching objective of tackling obesity at its roots, particularly within family settings. By educating individuals and families on healthy lifestyle practices and nutrition, these programs address immediate health concerns and contribute to building a more robust, productive, and healthier society.
Understanding strategies alone is insufficient without evaluating their broader economic effects. Successful interventions ultimately hinge on how short- and long-term costs and benefits balance across the healthcare system, the workforce, and local industries. Thus, we turn next to the economic implications of obesity prevention in Davidson County.
Economic Implications of Obesity Prevention
Short-term
Initial investments in education, policy development, and infrastructure changes. Immediate costs may be high, but are necessary to lay the foundation for long-term benefits. Some industries may face challenges (e.g., fast food), impacting livelihoods and operations, while others may see expansion (e.g., health and wellness sectors). Initially, healthcare expenditures in Davidson County may increase due to interventions being implemented, but over time, a decrease in obesity prevalence should reduce healthcare spending.
Long-term
A marked reduction in healthcare costs for treating obesity and its comorbidities should occur. Improved overall health can lead to increased productivity and economic growth. Healthier populations tend to be more productive, contributing positively to the economy. Redirecting towards healthier products and services encourages innovation and new market opportunities.
Yet, even the most cost-effective interventions cannot succeed in isolation. Political will, economic realities, and social dynamics deeply inform the implementation and sustainability of interventions. To fully grasp the potential as well as the challenges of obesity prevention, it is essential to consider the interplay of broader political, economic, and social factors.
Political, Economic, and Social Factors
A detailed interplay of political, economic, and social elements significantly influences the success of proposed interventions to address obesity in Davidson County. Understanding these factors is vital for effective implementation.
Government Policies.
Decisive government support can lead to effective policy implementation, funding, and enforcement. Political instability, changes in leadership, or shifting policy prerogatives can disrupt or deprioritise obesity interventions.
Industry Interests.
Cooperation with the food and beverage industry can lead to healthier product offerings and favourable public messaging. Resistance from industries that oppose obesity interventions, like fast-food chains or sugary drink manufacturers, may have a negative impact.
Public Awareness and Societal Attitudes.
Improved public awareness can influence societal pressure for change, affecting industry practices and government policies. Societal stigma towards obesity can lead to counterproductive or damaging policies. Misinformation and a lack of obesity understanding can also sabotage interventions.
Economic Factors.
Economic benefits like lowered healthcare expenses and improved productivity can inspire stakeholders. Initial costs of interventions might be a barrier, especially in economies facing fiscal restrictions.
Social Factors.
Community-based interventions can be effective, especially when they align with existing social structures and cultural norms. Social disparities and inequalities can impact the reach and effectiveness of interventions. For example, lower-income groups might have less access to healthy food or healthcare resources.
Taken together, these political, economic, and social dynamics underscore that interventions cannot succeed without structural change at the community level. Among the many pathways forward, tackling obesogenic food environments and addressing food insecurity emerge as the most urgent and foundational recommendations because, without addressing access to healthy, affordable food, other strategies are unlikely to achieve sustained impact.
Primary Recommendation: Obesogenic Food Environments and Food Insecurity
Addressing obesogenic food environments and food insecurity in Davidson County involves a complete approach with multiple agenda items (see Table 4).
| Agenda Item | Success | Challenge |
|---|---|---|
| Facilitate Access to Healthy Foods | Underwrite fruits, vegetables, and whole foods in low-income areas. Implement urban agriculture projects like community gardens. | Resistance from large food companies and modifying consumer habits rooted in convenience and fast food. |
| Regulate Fast Food Venues | Enforce zoning laws to limit fast-food venues near schools and low-income neighbourhoods. Impose higher taxes on unhealthy food alternatives. | Legal pushback from the fast-food industry and potential accusations of overstepping on consumer choice. |
| Education and Public Awareness Campaigns | Design comprehensive educational programs on nutrition and healthy eating habits starting in early school. | Overcoming misinformation and the pervasive marketing of unhealthy food options. |
| Strengthen Food Assistance Programs | Extend and enhance the reach of food assistance programs, ensuring they provide access to high-quality, nutritious foods. | Political antagonism to increased budget for social welfare programs and the stigma associated with accepting food assistance. |
| Encourage Food Industry Reform | Incentivise food factories to reformulate healthier and more nutritious products. | Balancing industry interests with public health goals and the technical difficulties in reformulating popular food products. |
Note. The table outlines agenda items, successes, and challenges in addressing obesogenic food environments and food insecurity in Davidson County.
Conclusion
Addressing obesity in Davidson County cannot rely on a single intervention. Instead, it requires coordinated efforts to reshape food environments, strengthen public education, expand access to nutritious foods, and foster accountability within the food industry.
If we succeed in these areas, we could lower healthcare costs, help people live better lives, and build a stronger local economy. Still, we face real challenges, including legal barriers, political hesitation, long-standing consumer habits, and pushback from the food industry.
The main takeaway is that no single approach, whether policy, education, or industry reform, can solve this problem on its own. Real progress will occur when these strategies and support align with ongoing investment and strong public backing.
Like Bruegel’s paintings, which depict the complex realities of his time, Davidson County’s approach to obesity should recognise that health depends on individual choices and the environments, economies, and social systems that influence them.
Note: This references list provides the primary sources from the original research paper submitted for the MSc in Global Healthcare Leadership (University of Oxford). Additional sources referenced in this article are accessible via embedded hyperlinks throughout the text.
References
Ameye, H., & Swinnen, J. (2019). Obesity, income and gender: The changing global relationship. Global Food Security, 23, 267–281.
Eskandari, F., Lake, A. A., Rose, K., Butler, M., & O'Malley, C. (2022). A mixed-method systematic review and meta-analysis of the influences of food environments and food insecurity on obesity in high-income countries. Food Science & Nutrition, 10(11), 3689–3723.
Herle, M., Pickles, A., Micali, N., Abdulkadir, M., & De Stavola, B. L. (2022). Parental feeding and childhood genetic risk for obesity: Exploring hypothetical interventions with causal inference methods. International Journal of Obesity, 46(7), 1271–1279.
Hurley, K. M., Cross, M. B., & Hughes, S. O. (2011). A systematic review of responsive feeding and child obesity in high-income countries. The Journal of Nutrition, 141(3), 495–501.
Jolliff, A. F., Moreno, M. A., & D'Angelo, J. (2020). The mediating role of depressive and anxiety symptoms in the association between obesity and problematic social media use in young adults. Obesity Science & Practice, 6(5), 454–459.
Oduro, M. S., Katey, D., Morgan, A. K., & Peprah, P. (2023). Problematic social media use and overweight/obesity: Explanatory pathway analysis of 124,667 in-school adolescents in 39 high-income countries. Pediatric Obesity, 18(11), e13073.
Okunogbe, A., Nugent, R., Spencer, G., Powis, J., Ralston, J., & Wilding, J. (2022). Economic impacts of overweight and obesity: Current and future estimates for 161 countries. BMJ Global Health, 7(9), e009773. https://doi.org/10.1136/bmjgh-2022-009773
Organisation for Economic Co-operation and Development (OECD). (n.d.). The heavy burden of obesity. Retrieved from https://www.oecd-ilibrary.org/sites/67450d67-en/1/2/1/index.html?itemId=/contentpublication/67450d67-en
Qiu, C., Hatton, R., Li, Q., Xv, J., Li, J., Tian, J., & Hou, M. (2023). Associations of parental feeding practices with children’s eating behaviors and food preferences: A Chinese cross-sectional study. BMC Pediatrics, 23(1), 1–12.
World Health Organization (WHO). (n.d.). Obesity. Retrieved from https://www.who.int/health-topics/obesity#tab=tab_1
World Health Organization. (2007). Prevention and control of noncommunicable diseases: Implementation of the global strategy: Report by the Secretariat. In Prevention and control of noncommunicable diseases: Implementation of the global strategy: Report by the Secretariat.
World Health Organization. (2021). Obesity and overweight. Retrieved December 19, 2023, from https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
Zamora, A. (2012). BMI calculator – Body Mass Index mobile calculator. Scientific Psychic. Retrieved from https://scientificpsychic.com/m/bmi-calculator.html

